Chimeric antigen receptor (CAR-T) therapy was first approved by the US FDA back in 2017 amid a great deal of fanfare and high expectations among patients about its potential as a revolutionary, perhaps even decisive, new pillar in the war on cancer. Five years later, however, many are still left wondering whether this radically different treatment paradigm can ever become the silver bullet the medical community has long been yearning for.
“Looking back, media coverage in the wake of the first American and European approvals was absolutely stunning in terms of coverage and attention, second only perhaps to the launch of Viagra and today’s roll out of COVID vaccines… Almost every top news outlet at the time seemed to be running front page stories on it in some shape and form,” recalls Karin Blumer, director of global patient engagement at Novartis Oncology.
This certainly had the benefit of giving much needed prominence to the unmet needs of cancer patients, but it also brought the disadvantage of whipping up a level of hype that was out of kilter with realities on the ground. “The clinical evidence is clear that certain hematologic malignancies do respond extremely well to CAR-T therapies, and it may yet prove to be a definitive treatment option, but certain elements of the media coverage made it appear as if practically any cancer could be cured using the cell and gene mechanism which is categorically not yet the case,” reflects Blumer.
Cutting through the Hype
Indeed, although treatment with CAR-T cells has certainly produced remarkable clinical responses in specific subsets of B cell leukaemia or lymphoma patients, many challenges continue to limit the therapeutic efficacy of CAR-T cells for solid tumours and haematological malignancies – not least severe life-threatening toxicities, modest anti-tumour activity, antigen escape, restricted trafficking, and limited tumour infiltration.

It initially proved tremendously difficult to dampen the soaring expectations for this new breed of medicines
“Sadly, with primetime TV news coverage in many countries focusing exclusively on sensationalist stories of instances where children seemingly doomed to die were making miraculous recoveries, it initially proved tremendously difficult to dampen the soaring expectations for this new breed of medicines,” says Blumer, though she does note that sustained engagement with professional patient advocacy groups is finally beginning to pay off and readdress the balance somewhat.
Claire Saxton, vice president of the Cancer Support Community, the largest professionally led non-profit network of cancer support worldwide, very much concurs. “Through telling patient success stories, it can sometimes seem like CAR-T is some sort of miracle cure for all. However, the brute reality today is it will only work with a specific set of patients and probably only have long-term positive impact for a third of that cohort. Therefore, while it is truly transformative for those patients where it succeeds, there are also those patients who relapse or who do not attain a good response and it is proper and ethical that these stories be transmitted too so as to not risk raising false hopes unnecessarily,” she explains.
Myth-Busting
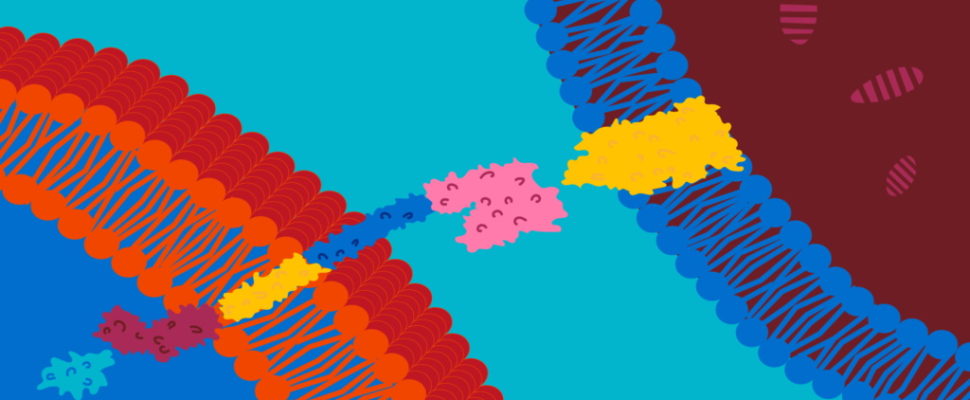
“The whole notion of CAR-T therapy certainly sounds futuristic to the uninitiated. Taking a person’s T Cells, modifying them to target cancer cells and putting them back in the body to hunt down and eliminate that cancer on their own is more the kind of story you’d imagine in a science-fiction novel so it’s hardly surprising that patients don’t realize that that future is now,” acknowledges Melanie Croce-Galis, director of US patient engagement at Novartis Oncology.
“Patients understand how chemotherapy works, because it’s been around far longer and almost everyone knows someone who has gone through it and what the potential side effects are. They also know that it takes several weeks and rounds of treatment. CAR-T, on the other hand, is the new kid on the block and so fresh that most people do not know much about it, including the fact that compared to chemotherapy it is a relatively straightforward experience and a one-time treatment with curative potential,” she opines.
Straight Talking
For Croce-Galis, the responsibility nonetheless lies with the companies pioneering these novel treatment paradigms to try to set the record straight wherever possible. “This is precisely what we at Novartis have been doing through awareness raising campaigns and collaborations with both patient advocacy groups and healthcare practitioners,” she assures.
“CAR-T therapies are undoubtedly a very powerful tool in treating advanced, aggressive blood cancers, but from the individual patient perspective, their full therapeutic benefit depends on many factors that need to be understood and put in context with other treatment options. One example is the overall fitness of a patient’s T-cells – a key success factor in CAR-T therapies,” agrees Marc Boutin, Novartis’ global head of patient engagement.
Let’s not forget there are still many unknowns with these very new treatments. For drug companies, dealing with cells rather than drugs is a real novelty; drugs have very clear specifications whereas with CAR-T we are talking about living organisms where the dose of cells is never the same. It all depends on how many cells you can collect, how many can be successfully transduced with genetic procedures, how many expand in the patient, and how many stay active in the patient over time. In short, there’s a strong element of uncertainty,” stresses Nicolaus Kröger, president of the European Society for Blood and Marrow Transplantation (EBMT).
“As the science and medicine is complex, patient advocacy groups play a central role in this area and for us and other sponsors, this space is a sensitive area and requires utmost responsibility. It is absolutely imperative we manage to strike the right balance between providing accurate information on a transformative therapy and the responsibility to manage expectations for patients whose cancer cannot be treated with CART therapies,” reaffirms Boutin.
A Reality Check
What then, does the current outlook hold for this pioneering and exciting class of medicines? “Right now, CAR-T is the definitive and curative answer for some patients, but not all. We still see a significant number of patients that are either not responsive or relapsing, usually within the two-year mark. The question is therefore how can we do a better job of figuring out which treatment is best for which patient and what order we should be progressing through these treatments to take the best advantage of what is currently available,” reveals Lorna Warwick, CEO of the Lymphoma Coalition, a worldwide network of patient groups with a full or partial focus on providing support to patients with lymphoma.

Right now, CAR-T is the definitive and curative answer for some patients, but not all
“In my opinion, there is still a great deal of research to be done around how the state of a patient’s T cells impacts their response to a CAR-T therapy and whether we should be harvesting T cells earlier in the treatment paradigm in case of a relapse later. And it’s not just from the clinical trials investigating these things, that we will secure these answers, but also from a growing pool of real-world evidence that we need to start processing,” she argues. At this moment in time, there are many relapsed/refractory patients wondering whether there are any treatments left for them and it is our moral obligation to conduct more research into figuring out precisely how to cure them,” insists Warwick.
“Initially, we were all swept up, myself included, in a wave of excitement about CAR-T and the amazing effect that it had on patients who had been through fifth-, sixth- or seventh-line therapies with no response,” recounts Navin Pinto, associate professor of paediatrics at the University of Washington School of Medicine and an attending physician at Seattle hospital who was brought in at an early phase to evaluate if cell and gene technology would work for other malignancies and fight other cancers, solid tumours, nervous system malignancies, and leukaemia.
His overall assessment is mixed. “Expanding the use of CAR-T beyond CD19 has been a significant challenge, for several reasons. The patients I meet are oftentimes not on their second or third line of treatment, but on their fourth, fifth, or sixth; they are looking for any possible therapies and know that their cancer has no known cure. Moreover, the same ‘home runs’ that were seen with CD19 have not yet been witnessed for other types of cancer; we have treated hundreds of patients with solid tumours without the same miraculous response even though there have been hints in many clinical trials of extraordinary responders,” he admits.
Encouraging Signs
Nevertheless, Dr Pinto still has high hopes for the future having noticed that many CAR-T patients are exhibiting partial responses, such as a prolongation of disease stability, and hints of immuno-activation. Many experts in the CAR-T field believe that this suggests an engineering problem that can be potentially fixed by better equipping the T cells to more robustly handle tumours through unique target selection which limits their exhaustion of repetitively fighting a cancer cell.
“There are multiple rounds of manufacturing that probably still need to be addressed. The first is the actual construction of the CAR. This is a completely artificial construction and usually introduced into T cells with viruses. The genetic signal for this CAR-T is not a structure that necessarily exists in nature. They are taking components of the immune system, and assembling them together like building blocks, to make a new protein that can recognize a tumour and evade the immune system to target it. The building blocks that are selected to make a CAR are very important and very minor adjustments in the building blocks have led to major differences in the T cells’ ability to withstand exhaustion,” reasons Pinto. “For a given malignancy or given target, unfortunately, it is not the same pattern of building blocks that worked for CD19, so there’s a lot of research still to be done, but equivalent solutions are probably out there waiting to be uncovered,” he concludes.

I think [CAR-T therapies] will be used for earlier disease stages, where they might not only be more effective but would also reach larger patient populations
“I would say cell and gene therapies will never become mainstream like, say, medication for hypertension or antibiotics, for instance. I suspect it will be for specific groups of patients, perhaps mainly for haematological malignancies. But I do think they will be used for earlier disease stages, where they might not only be more effective but would also reach larger patient populations,” predicts Nicolaus Kröger.
Another element of managing expectations relates even to those eligible for this new class of treatment. “Unfortunately, I encounter many instances where patients that come in are eligible for CAR-T, and one month later, when their cells are ready, they are too sick to receive treatment. That is often the scariest prospect and probably where pharma will have some role in shortening the manufacturing time. We need to think about how to provide off the shelf therapies so that we do not have to collect the cells from everybody and can make a more feasible and widely applicable therapy for patients,” urges Pinto.
A Marathon, not a Sprint
Nonetheless, there are still plenty of irons in the fire. For example, a reversion to allogenic treatments might ultimately herald a breakthrough in the quest to finally get CAR-T delivering on its tremendous promise. “To date, the focus has pretty much been exclusively on autologous CAR-T therapies, where the patient’s own T-cells are extracted and manipulated, which is protracted process that sometimes takes too long for late-stage cancer patients. Allogeneic CAR-T therapies, by contrast, are more of an ‘off-the-shelf’ set of therapies, in the sense that they can be manufactured ahead of time. They are more complex to engineer because genome editing needs to be done to avoid host rejection, but it’s theorized that because the T-cells come from healthy donors, they might be less depleted than the T-cells extracted from cancer patients,” surmises Kröger.
And for Peter Marks, director of the Centre for Biologics Evaluation and Research (CBER) of the US FDA, there are still a multitude of reasons to remain optimistic. “For cell-based therapies, primarily CAR-T cells, we’ve seen tangible progress in manufacturing and development. Candidates are more routinely progressing through the development process, and now we’re starting to register multiple approvals per year, branching out from just the one hematologic target, CD19 which is really quite impressive!” he reassures. “For sure we’re starting to bump into some toxicities, but that is all part and parcel of the process and we’re equally witnessing robust progress in terms of positive clinical trial data results.”
While counselling the need to temper expectations for the existing patient population Dr Marks is quietly confident that, with time, cell and gene therapies will take their place as one of the most impactful medical breakthroughs of our epoque. “On the horizon are other hematologic targets, as well as, potentially, solid tumours — especially as we start to look at allogeneic CAR-T cells, not to mention technologies such as directly administered or in vivo genome editing, which, once we get over the issues of off-target effects, could be thoroughly transformative,” he enthuses.